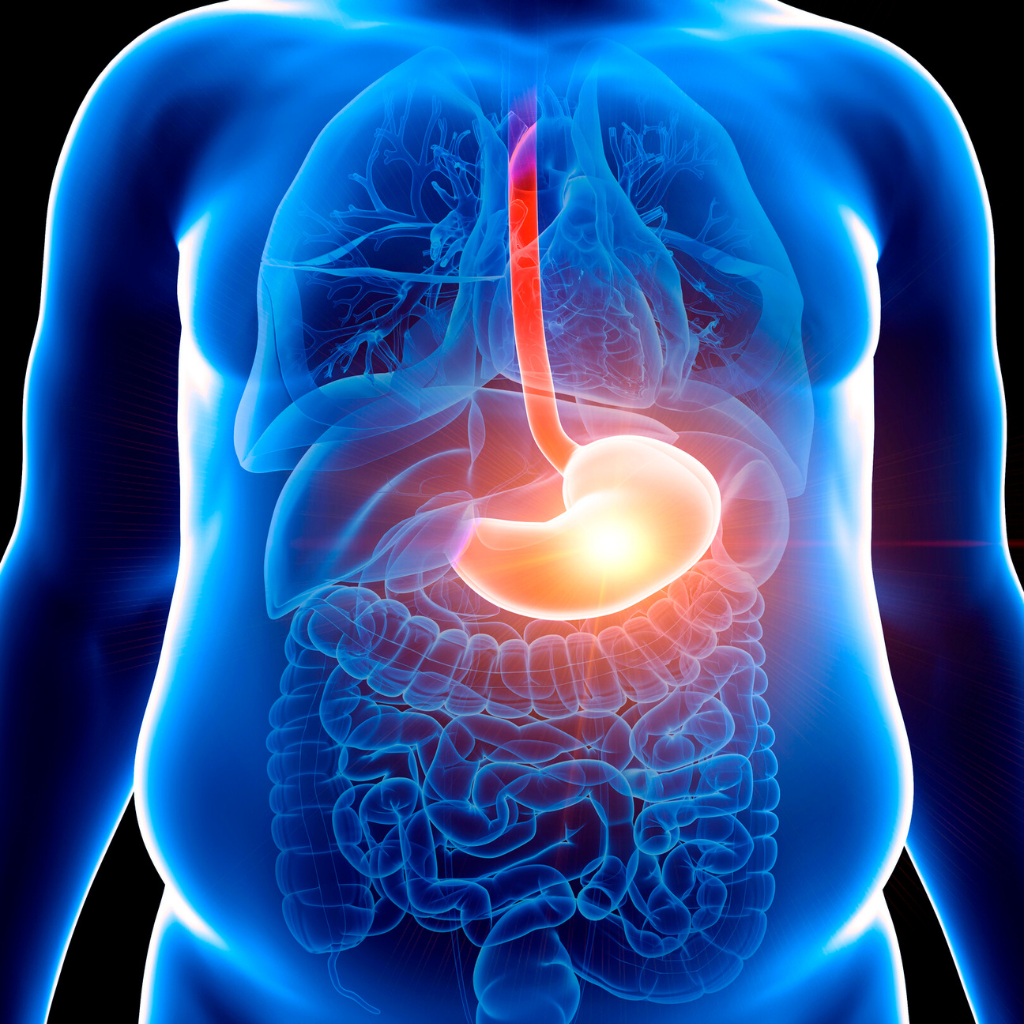
Esophageal cancer is a type of cancer that originates in the esophagus, which is the muscular tube that connects the throat to the stomach. The esophagus is responsible for transporting food and liquids from the mouth to the stomach for digestion.
The actual treatment plan for esophageal cancer will depend on various factors including the stage of the cancer, the patient’s overall health, and individual preferences.
Surgery is the most common treatment option for localised esophageal cancer, ie for tumours that haven’t spread to distant parts of the body. The type of surgery performed depends on the location of the tumour, its size, and the stage of the cancer. Here are some surgical approaches used in the treatment of esophageal cancer:
Surgery for esophageal cancer is a major procedure that requires careful evaluation of the patient’s overall health and the extent of the cancer. Often, pre-surgery treatment, also known as neoadjuvant treatment, can be utilized to down-stage the cancer, decrease the size, and improve the outcomes of surgery. Neoadjuvant treatment involves the use of radiotherapy and/or chemotherapy.
Radiotherapy, also known as radiation therapy employs high doses of radiation to target and eliminate cancer cells. Here’s an overview of how radiation therapy is utilized in the treatment of esophageal cancer:
Radiation therapy for esophageal cancer is a highly targeted procedure, aiming to maximize the impact on cancer cells while minimizing harm to healthy surrounding tissue. The treatment plan is customized to the patient’s specific condition, including factors like the stage and location of the cancer, as well as the individual’s overall health.
Chemotherapy is a significant treatment approach for esophageal cancer, particularly in cases where the cancer has spread beyond its original site or when it’s part of a multimodal treatment plan. Chemotherapy involves using anti-cancer drugs to target and destroy cancer cells throughout the body. Here’s an overview of how chemotherapy is utilized in the treatment of esophageal cancer:
The specific chemotherapy drugs used and the treatment schedule depend on various factors, such as the cancer’s stage, the patient’s overall health, and any previous treatments received.
Targeted therapy is a significant advancement in the treatment of esophageal cancer, particularly for cases that involve specific genetic mutations or molecular characteristics. This approach involves using drugs that specifically target certain molecules or pathways involved in the growth and spread of cancer cells. Here’s an overview of how targeted therapy is employed in the treatment of esophageal cancer:
It’s important to note that targeted therapy is not suitable for all esophageal cancer cases. The decision to use targeted therapy depends on the results of molecular testing and the presence of relevant targets in the cancer cells.
Immunotherapy is an approved treatment of esophageal cancer, claimable under the Ministry of Health Cancer Drug List. It is approved for use in the adjuvant setting, following completion of neoadjuvant chemotherapy and radiation and surgery, or for the use in advanced esophageal cancer, that has spread to other organs.. This approach harnesses the body’s own immune system to recognize and fight cancer cells. Here’s an overview of how immunotherapy is employed in the treatment of esophageal cancer:
It’s important to note that not all patients with esophageal cancer will be candidates for immunotherapy, and its use often depends on factors such as the cancer’s molecular characteristics and the overall health of the patient.
Undergoing surgery for esophageal cancer can lead to several potential side effects. These side effects can vary depending on the extent of the surgery, the patient’s overall health, and individual factors. Here are some common side effects associated with esophageal cancer surgery:
Radiation therapy for esophageal cancer can lead to a range of side effects, as the treatment aims to target cancer cells while affecting some healthy tissue in the area. These side effects can vary in intensity and duration depending on factors such as the radiation dose, the treatment area, and the patient’s overall health. Here are some common side effects associated with radiation therapy for esophageal cancer:
Chemotherapy for esophageal cancer can lead to a variety of side effects, as the treatment involves using powerful drugs to target and destroy cancer cells. These side effects can vary in severity and duration depending on the specific chemotherapy drugs used, the treatment regimen, and the patient’s overall health. Here are some common side effects associated with chemotherapy for esophageal cancer:
Targeted therapy for esophageal cancer can bring about specific side effects, as this treatment approach focuses on targeting particular molecules involved in cancer growth. The severity and occurrence of these side effects can vary based on the specific targeted therapy drug used, the patient’s individual response, and their overall health. Here are some common side effects associated with targeted therapy for esophageal cancer:
Immunotherapy for esophageal cancer can lead to various side effects, as this treatment approach harnesses the immune system to target cancer cells. The occurrence and intensity of these side effects can differ based on the specific immunotherapy drug used, the patient’s individual response, and their overall health. Here are some common side effects associated with immunotherapy for esophageal cancer:

It is important to remember that esophageal cancer can be treated successfully if caught early. If you have any concerns about your esophagus health or notice any changes, do not hesitate to see a healthcare professional for evaluation.
If you suspect that you or your loved one have esophageal cancer, it is advisable to get the support you need. Early detection and diagnosis of esophageal cancer is key to treating the disease.
Regardless of what stage your esophageal cancer may be at, you should schedule an appointment to see an oncologist specialising in esophageal cancer as soon as possible. With the speed of developments in esophageal cancer diagnosis and treatment, novel emerging treatment options could be explored by your oncologist.

Esophageal cancer is a type of cancer that originates in the esophagus, which is a muscular tube that connects the throat (pharynx) to the stomach. The esophagus plays a crucial role in the process of swallowing, by transporting food and liquids from the mouth to the stomach for digestion.
Esophageal cancer typically develops from the cells that line the inner surface of the esophagus. There are two main types of esophageal cancer:
Early detection and timely treatment are important for improving the prognosis and outcomes for individuals with esophageal cancer. It’s advisable for individuals at risk or experiencing symptoms to seek medical attention for proper evaluation and diagnosis.
Esophageal cancer is the eighth most common cancer worldwide. The two main histological types of esophageal cancer, adenocarcinoma and squamous cell carcinoma, have different prevalence patterns. Adenocarcinoma is more common in Western countries, while squamous cell carcinoma is more prevalent in areas with high rates of tobacco and alcohol consumption.
Esophageal cancer is less common in Malaysia as compared to other parts of the world. Esophageal cancer accounted for 1% of all cancer cases in Malaysia between year 2012-2016. Esophageal cancer is often diagnosed at an advanced stage in Malaysia, which can impact treatment options and outcomes. The incidence rate and mortality rate for esophageal cancer might be influenced by factors such as lifestyle and genetics.
Signs and symptoms of esophageal cancer can vary, and some individuals may not experience any symptoms in the early stages.
It’s important to note that these symptoms can also be caused by other conditions, and experiencing one or more of these symptoms doesn’t necessarily mean a person has esophageal cancer. However, if you or someone you know is experiencing persistent or worsening symptoms, especially difficulty swallowing or unintended weight loss, it’s important to consult a healthcare professional for proper evaluation and diagnosis. Early detection and treatment can significantly impact outcomes for esophageal cancer.
Screening for esophageal cancer is typically recommended for individuals who are at a higher risk due to certain risk factors, such as a family history of the disease or certain medical conditions.
It’s important to emphasize that decisions about screening should be made in consultation with a healthcare provider. They can assess your individual risk factors, medical history, and symptoms to determine whether screening is appropriate for you.

Esophageal cancer is diagnosed through a combination of medical history assessment, physical examination, imaging tests, and tissue sampling. The diagnostic process is aimed at confirming the presence of cancer, determining the stage of the disease, and guiding treatment decisions. Here’s an overview of how esophageal cancer is diagnosed:
Diagnosing esophageal cancer involves a multidisciplinary approach, with input from various healthcare professionals such as gastroenterologists, oncologists, radiologists, and pathologists. It’s important to have open and thorough discussions with the medical team throughout the diagnostic process to ensure you understand your diagnosis, its stage, and the recommended treatment options.
The development of esophageal cancer is influenced by a combination of genetic, lifestyle, and environmental factors. While the exact causes of esophageal cancer are not always fully understood, certain risk factors have been identified that increase the likelihood of developing the disease. Here are some common causes and risk factors associated with esophageal cancer:
It’s important to note that having one or more risk factors doesn’t guarantee the development of esophageal cancer, and some individuals without these risk factors might still develop the disease. Reducing modifiable risk factors like tobacco use, excessive alcohol consumption, and maintaining a healthy diet can help lower the risk.

Esophageal cancer can be categorized into two main types based on the specific cells that become cancerous within the esophagus. These types are defined by their histological characteristics and can have different risk factors, locations within the esophagus, and treatment approaches. The two primary types of esophageal cancer are:
Less common types of esophageal cancer include:
The distinction between adenocarcinoma and squamous cell carcinoma is important because they have different risk factors, presentations, and potential treatment approaches. Proper diagnosis and determination of the specific type of esophageal cancer are crucial for guiding the most effective treatment plan.
Esophageal cancer staging is a system used to describe the extent of the cancer’s spread within the body. Staging helps determine the best treatment approach and provides insight into the prognosis. The most used staging system for esophageal cancer is the TNM system, which stands for Tumour, Node, and Metastasis. This system classifies the cancer based on the size of the tumour, the involvement of nearby lymph nodes, and whether the cancer has spread to distant parts of the body. The stages are typically numbered from 0 to IV, with subcategories indicating the extent of each factor. Here’s an overview of the general stages:
Abnormal cells are found only in the innermost layer of the esophagus lining and have not invaded deeper layers.
The cancer is limited to the inner layers of the esophagus and might involve nearby lymph nodes. It has not spread to distant parts of the body.
The cancer has grown into deeper layers of the esophagus or nearby tissues, and lymph nodes may be involved. It still hasn’t spread to distant parts of the body.
The cancer has invaded nearby structures, such as the trachea, bronchi, aorta, or heart. It may have spread to nearby lymph nodes.
The cancer has spread to distant parts of the body, such as the lungs, liver, bones, or other organs. Stage IV is further divided into IVA and IVB, based on the extent of the spread.
Staging might also include additional factors such as the location of lymph node involvement, the number of affected lymph nodes, and specific characteristics of the tumour.
Site Map | PDPA | Terms of Use | Disclaimer |
Contact Us | Career | Media Contact